Today, nothing can be achieved without the support of the Internet. That is also true when it comes to creating your photography business. In the 21st century, odds are huge that new customers will find you via a Google search, a picture shared on Instagram, or a positive comment left by their friends on Facebook. Wait a second! Do not be scared by those very elaborate, and somehow remarkable, brands. The tools they provide are mostly free and quite simple to use.
Very soon, you will be prepared to play together, experiment and eventually spread your wings and fly. Then, you will quickly see new visitors flowing onto your photography site. All you need are your first developed notions. That is where we step in, with this detailed guide. Here are the best free tools to promote your photography business online.
1. Create your unique photography website
Make it your dwelling. Your photography website, too called your online portfolio, is the  area where people can find who you are and what you’re doing at any given moment. As it has been the most convenient manner, you put your URL (online address) everywhere, from the social accounts to your own business cards which you hand to your customers. It goes without saying, but this web design should look impeccable. It will inspire your customers and say a lot about your professional practice to prospective new customers.
area where people can find who you are and what you’re doing at any given moment. As it has been the most convenient manner, you put your URL (online address) everywhere, from the social accounts to your own business cards which you hand to your customers. It goes without saying, but this web design should look impeccable. It will inspire your customers and say a lot about your professional practice to prospective new customers.
Do not know where to begin? You can confidently turn to Wix, a solution accepted by thousands and thousands of photographers worldwide. Easy to master yet, offering the most sophisticated features, it satisfies the requirements of photographers to have an exceptional site — one that looks like no other and is telling of their artwork. Create your account in one click, add the Wix Pro Gallery, place your name and practice in large on the homepage, and make a contact form to get your business rolling. Finally, ensure that your photography website is truly mobile-friendly, and you are ready to go!
2. Do your Search Engine Optimization
You have read and heard a lot about those words, SEO? These 3 simple letters (which stand for Search Engine Optimization) may be the most effective instrument for the photography business to succeed online. Fundamentally, SEO means working on your site to be certain that Google, Bing and their friends will easily find it and rank it at a high position whenever individuals are searching for your activity. Some areas are more aggressive than others: let us consider a “Boudoir photographer at Duluth” (229,000 outcomes), far less crowded than a “Landscape photographer in Los Angeles” (6,180,000 outcomes). However, the principles remain the same.
Namely: make sure you discover the right key words, the ones that a client searching for a business like you’re very likely to type in their favourite search engine, a small business coach may be able to help you on this. As soon as you have them, be sure they are clearly on your URL, your page titles and your search engine optimization title. Last, because no photography site is complete without a complete gallery of pictures, why not maximize these last ones also? Insert the alt-text into each and every picture to maximize your chances available not only on Google, but also on Google Images.
3. Start a site
A blog is a fantastic way to interact with customers or individuals interested in photography and make them understand your company better. It is also the anteroom to your photography site, to which it contributes through judicious clickable links — added in the header, the content or the footer of your site. In terms of the technicalities, Wix makes it super simple to make a killer site you will connect in a single click to your website. The only difficulty? Writing web page content. Like most photographers, you are probably more comfortable with a set of lenses than you are with a computer keyboard — or God forbid, a pencil!
Worry no more: generating written content is simpler than you think. Do not forget that a blog is intended to share yourself on a casual level. The text needs to be less commercial than your website. You can also set yourself as an authority and one of the top business advisors in your field. For Instance, if you are specialized in travel photography, you can write about “The Gear You Need to Always Carry with You”, “How to Traveling on a Low-Budget and High Definition” or “Light 101: The Guide for Shooting in Sunny Destinations”. For a larger impact, do not forget to add stunning images to your text, and even short movies as a result of this new (and extremely powerful) Wix Video.
4. Send great old newsletters
The email, an artefact in the 20st century? Think again. Today more than ever, companies — big, small and middle — reach out to their customers using written messages. And there is good reason for this: email is 40 times more capable of obtaining new customers than Facebook or Twitter. A newsletter could be an exceptional way to market your photography business, or get more exposure for your own creations. You’ve got loads of events to engage your community, from New Year wishes to your most recent blog post, to a customer’s birthday or a promotional offer for wedding photos.
A couple of rules must be considered. First, a gorgeous layout is an absolute must, and will substantially increase the success of your mails. Simply get Wix ShoutOut, an easy-to-use and free alternative for your newsletters. You decide on the template that suits your aesthetics the most, you upload your images and place your sales copywriting, and it is a done deal! Second, ensure that your content is relevant for the readers you’re sending it to. You might not want to send your most recent wedding photography package to the happily married couples in your database? Segment this last one as far as possible, to increase the relevancy — and therefore, the success — of your own campaigns.
5. Master the power of social media
In 2018, to be able to effectively market your photography company, being present and active on social networks is an absolute must. The platforms are based on the same principle (building a community you will share your articles with), but places the stress on various mediums. As you’re a photographer, ideally, you’ve got a collection of beautiful pictures to select from, and that will work well on all types of social platforms. These can be divided in two classes. The first is composed of the overall social media, used by everyone — such as Facebook (two million users!), Twitter, Pinterest and Google+. The next group is the photography-specialized platforms, including, Instagram, 500px or FlickR.
Whichever social networking channel you choose to spend In, there are a few general rules you ought to know. First, post frequently (once or twice per day on Facebook, twice per day on Instagram, etc.) but not spam your neighbourhood with enormous posts. Second, whatever the platform, don’t forget to add a caption (a brief text) with your picture, to be able to raise the reach and the participation. Finally, use the perfect hashtags for more eyes on your articles.
6. Experiment PPC marketing
This instrument is the only one that is not for free. But the cash is very little and the return on investment is simply sensational. Advertising has always been a must for photographers just like any other organization. But in 2018, we are not referring to the Mad Men manner (fancy advertisers with fancy slogans and fancy suits) anymore. On the contrary: PPC (Pay-Per-Click) advertising is all about doing it yourself. Whether Facebook or on Google, the point is to set your content online, and to pay just for the actual clicks you’ve received.
To run a successful AdWords campaign, you first need to find the ideal target audience. It should be people which may be interested in your services (for cases, people in their 20s and 30s living locally in Melbourne, Australia, if you are one of the best wedding photographers in Melbourne). Then, you want to make the content. It needs to be straight to the point, with a very clear CTA (call to action), like “Discover my deal!” or “Buy now!”. Step number 3: pick the budget that you need to allocate to your effort. It is good practice to begin with a little bit of money, and raise the stakes when you find the very first clients coming in. Finally, keep your eye on your metrics after the effort is completed. It’s the ideal way to make the next campaign even better than the preceding one.
7. Get featured on picture blogs
Many excellent photography sites open their pages to talented photographers, for them to flaunt their images and reach a new audience. Needless to say, your images should be engaging or unique enough to catch the eyes of the sites’ editors. If you’re actually selected, it is free advertising for your photography that you don’t want to miss.
Discussing quality sites, the Wix Photography Website (at your service) is happy to collect and exhibit the work of awesome Wix photographers. Think no more and discuss! Be it as a post on the Wix FB page, a tweet or a complete interview on the website, they are delighted to showcase your work to their community which will definitely help to boost the sales management process.
8. Register on online directories
Directories and listing websites like Bing Places, the Yellow Pages or Yelp are go-to areas that people often turn to so as to discover a business in their geographic location. If you take weddings, events, newborns, portraits or boudoirs, they ought to be among the first places to market your photography business.
Let’s say you have a physical studio, do not forget to add its address and details into Google My Business. In this way, when people will find you on their Google results, they won’t only see your site, but also a map with your location, your work hours and contact on the ideal strip of the page. It looks like a little change, but it really can radically boost your conversions!
9. Input photo contests
It is a great and, most of the time, a free solution to place your name and photography in the spotlight. Countless great contests are running throughout the year on web, for every possible genre or degree of photography. Needless to say, just a few make it to the top. However, on the way to it, you’re going to get many chances to get showcased by magazines or blogs. Plus, the adrenaline brought on by competitions that pumps through your veins may only benefit your imagination. Curious?
10. Personalize your emails’ signature
Your signature is the fastest and most discreet way to spread your name. Most of today’s inboxes offer you the chance to celebrate the signature that will appear automatically at the bottom of all your electronic messages. Ensure you add your brand, specialties and contact, in addition to a link to your social networks along with your photography website so when you email important people like business management specialists, they can refer you. Who said that online marketing was challenging?










































 area where people can find who you are and what you’re doing at any given moment. As it has been the most convenient manner, you put your URL (online address) everywhere, from the social accounts to your own business cards which you hand to your customers. It goes without saying, but this web design should look impeccable. It will inspire your customers and say a lot about your professional practice to prospective new customers.
area where people can find who you are and what you’re doing at any given moment. As it has been the most convenient manner, you put your URL (online address) everywhere, from the social accounts to your own business cards which you hand to your customers. It goes without saying, but this web design should look impeccable. It will inspire your customers and say a lot about your professional practice to prospective new customers.
 Use powerful paper. This will be more expensive, but strong paper lasts longer and gives a better sense of professionalism. It shows people that you take your art seriously enough to invest in a great quality business card. Strong paper also tends to keep color better, which will make your art look great! In case you really want to show off your 50 great paintings, then publish 50 great distinct business cards and let people chose which business card they would like to choose from you.
Use powerful paper. This will be more expensive, but strong paper lasts longer and gives a better sense of professionalism. It shows people that you take your art seriously enough to invest in a great quality business card. Strong paper also tends to keep color better, which will make your art look great! In case you really want to show off your 50 great paintings, then publish 50 great distinct business cards and let people chose which business card they would like to choose from you.




 As Handler and Horan had little experience with exhibitions and weddings, they partnered with Michelle Gomez, a modern curator who conducts Creative Unions; an event planning company designed to incorporate contemporary art into parties, and with Carlyn Thomas, curator in Terrault Contemporary to plan every detail, including a nationwide call for entry requesting for homosexual, Miami, wedding, and Golden Girls inspired art. A few of the items used during the wedding included the Leah Guadagnoli’s and Frank Stella-meets-home products terracotta relief sculptures, which join pastel beach house décor with natural late 80s assemblage. For the exhibitions decor, Alex Ebstein’s collaged yoga mats of horizontal Matisse-esque shapes of hot pink, teal, and white sign in Miami in the ’80s, but also aestheticize present exercise culture. A mirror sculpture, which was neon lined by Esther Ruiz floats on an oblong hot pink glow on the wall around it, offering an abstract window into another world where geometric principles govern was also designed for the couple to be. The wedding altar was designed especially for the grooms by Anya Mizani and is among the most dramatic pieces in the series. It comprised of a human-sized pink neon rectangle, it is full of big, faux tropical leaves in green and glistening gold. Not only an altar for the ceremony, this piece reinforces the stunning spectacle of the wedding for a performance.
As Handler and Horan had little experience with exhibitions and weddings, they partnered with Michelle Gomez, a modern curator who conducts Creative Unions; an event planning company designed to incorporate contemporary art into parties, and with Carlyn Thomas, curator in Terrault Contemporary to plan every detail, including a nationwide call for entry requesting for homosexual, Miami, wedding, and Golden Girls inspired art. A few of the items used during the wedding included the Leah Guadagnoli’s and Frank Stella-meets-home products terracotta relief sculptures, which join pastel beach house décor with natural late 80s assemblage. For the exhibitions decor, Alex Ebstein’s collaged yoga mats of horizontal Matisse-esque shapes of hot pink, teal, and white sign in Miami in the ’80s, but also aestheticize present exercise culture. A mirror sculpture, which was neon lined by Esther Ruiz floats on an oblong hot pink glow on the wall around it, offering an abstract window into another world where geometric principles govern was also designed for the couple to be. The wedding altar was designed especially for the grooms by Anya Mizani and is among the most dramatic pieces in the series. It comprised of a human-sized pink neon rectangle, it is full of big, faux tropical leaves in green and glistening gold. Not only an altar for the ceremony, this piece reinforces the stunning spectacle of the wedding for a performance.
 -Promotes Self Expression
-Promotes Self Expression
 background can add a decorative element to what’s basically a pared-back style.
background can add a decorative element to what’s basically a pared-back style.
 to help keep your prized pieces safe is to set up distractions around the house so the kids are not focused on playing with your ceramic sculptures. Try a music room or other play rooms that will keep the kids entertained without the temptation of touching the art.
to help keep your prized pieces safe is to set up distractions around the house so the kids are not focused on playing with your ceramic sculptures. Try a music room or other play rooms that will keep the kids entertained without the temptation of touching the art.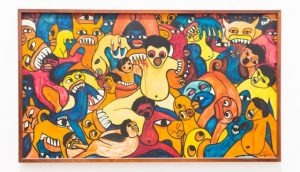 Turner also suggests going a step further by incorporating color. Brightly colored abstract artworks or figurative art not only bring sophistication to your home, but they can also enliven a space, making it cheerful and delightful to young children, Turner says. Children like to engage and be visually stimulated, so why not appeal to their budding love for culture and the arts by introducing brilliant pops of art? They may be young, but kids really do recognise quality design early. To complement high-end pieces, you might also consider showcasing children’s art also, it’s a great juxtaposition and conversation starter.
Turner also suggests going a step further by incorporating color. Brightly colored abstract artworks or figurative art not only bring sophistication to your home, but they can also enliven a space, making it cheerful and delightful to young children, Turner says. Children like to engage and be visually stimulated, so why not appeal to their budding love for culture and the arts by introducing brilliant pops of art? They may be young, but kids really do recognise quality design early. To complement high-end pieces, you might also consider showcasing children’s art also, it’s a great juxtaposition and conversation starter.



 Meanwhile at Cable Beach, a dinosaur on the move has finally landed. Andy Greig’s “Zika” sculpture has actually been on display around Broome since winning the Shinju Matsuri A View to Asia Art Award last September and is now dominating the Cable Beach renown for
Meanwhile at Cable Beach, a dinosaur on the move has finally landed. Andy Greig’s “Zika” sculpture has actually been on display around Broome since winning the Shinju Matsuri A View to Asia Art Award last September and is now dominating the Cable Beach renown for 




 The clothes hamper in the main restroom is a multi-color gambling establishment slots. The living-room CD cabinet is an old-fashioned, intense red-and-white Coca-Cola dispenser. A wall light was as soon as a gas pump.
The clothes hamper in the main restroom is a multi-color gambling establishment slots. The living-room CD cabinet is an old-fashioned, intense red-and-white Coca-Cola dispenser. A wall light was as soon as a gas pump.

